What Is Histamine & Why I Can’t Stand It
When we think of histamine what comes to mind is runny noses and itchy eyes in the spring and maybe getting hives. Histamine is actually a bigger part of all of our lives going well beyond hay fever and allergies.
Histamine is an important part of our local immune system when we react to something like a bee sting or pollen or a peanut. It is stored in mast cells (immune cells) and basophils (a type of white blood cell) and when we have an injury or insult, the cell dumps those contents and cause blood vessels in the area to basically leak getting important immune cells to the area. This creates the typical swelling and puffiness we see with something like a hive or swollen red eyes with allergies. Histamine also causes itching.
But it also is an important neurotransmitter in the brain as part of our sleep-wake cycle (why some anti-histamines make you sleepy) as well as how we perceive pain, body temperature regulation and hormone balance. Histamine also acts as a neurotransmitter in the uterus and appears to play a role in sexual arousal and erections. It is also active in the gut particularly in that it stimulates parietal cells in the stomach to secrete stomach acid and plays a role in gut motility.
And for you women with autoimmunity note that histamine appears to play a role in differentiating T-cells which modulate your immune system when all goes well. Histamine receptor blockers are being studied currently for treatment of Multiple Sclerosis….interesting right? Something to consider all my ladies with PCOS and Hashimoto’s as well.
Get you FREE copy of my Guide To Lab Testing & Your Hormones
This guide covers hormonal testing and thyroid patterns and will show you how to suss out the Hormonal Dealbreakers of inflammation, anemia and blood sugar problems.
Get Your Free Lab Guide HereClearly, we need histamine as part of normal physiology but why does it makes some of us miserable?
Again, there’s the classic allergy picture where we have become sensitized to allergens and have an over-zealous response to pollen, grass, dust, etc. and suffer with runny noses and itchy, watery eyes. There’s also the classic food allergy where we eat the strawberries and get hives or the peanut and go into anaphylaxis. But there’s also a lot of other misery we can get when we can’t manage histamine properly.
What Is Histamine Intolerance?
This is the recent hell I have been in but thankfully it’s under control now! In short, histamine intolerance can develop when you are unable to clear out histamine related to our diet or if you’re having an exaggerated histamine release in your body.
An excessive build up of histamine can be caused by many things ranging from infections (commonly gut pathogens and infections like SIBO, small intestine bacterial overgrowth), overzealous mast cells (mastocytosis or mast cell instability) dumping histamine too often and inappropriately or it can come from filling up your histamine bucket faster than you can dump it. By this I mean the mechanisms and enzymes that normally clear out histamine from your system whether it comes in from food or as the result of an infection are running sluggish. This can be due to genetic variances in these enzymes (as is the case with myself) or any number of reasons we’ve slowed that enzyme or drained it’s cofactors and now it’s running too slow to keep you out of histamine side effects.
Symptoms of Histamine Intolerance
Any of the following may have histamine as a culprit and you do not need to have all on this list by any means to have a histamine issue:
- Itching
- Irritability
- Insomnia
- Menstrual irregularities – abnormal cycle timing, excessive cramping
- Headaches (more extreme cases: migraines, seizures)
- Flushing
- Rapid heart beat
- Profuse sweating
- Seasonal or food allergies
- Urticaria or prickly heat
- Exaggerated response to mosquito bites (large, very swollen, very itchy)
- Runny nose or bloody nose
- Car sickness, motion sickness and sea sickness
- Nausea, vomiting, stomach pain or loose stools
- Know gut infections such as candida, SIBO, etc.
- Chronic viral issues such as EBV
- GERD or heartburn
- Asthma (classic and exercise induced)
- Chest tightness or shortness of breath
- Increased sex drive and libido
- Skin issues including acne, hives, eczema and psoriasis
How Do We Get Histamine Intolerance?
There are many reasons this issue can develop and I never imagined so many women in my practice would be dealing with this when I graduated a dozen years ago – let alone myself.
Here are a few reasons for histamine intolerance:
Genetic Susceptibility due to SNPs SNPs (single nucleotide polymorphisms meaning a single DNA base is swapped for another creating less enzyme efficiency). More on this in this podcast with Dr Ben Lynch.
Remember though that gene SNPs are just one reason an enzyme may be sluggish, many lifestyle factors (called epigenetics) will affect enzyme efficiency so even if you have a SNP related to an enzyme you can get better function by cleaning up the environment that the gene and enzyme live in. For example, we know there are many things that slow an enzyme down such as oxidative stress and that enzymes need cofactors in order to work and these nutrients can be deficient (B vitamins and minerals like magnesium are common cofactors for many enzymes). We can affect a gene’s function by decreasing exposure to things that slow them down and ensuring adequate cofactors. This applies whether there is a SNP or not.
If your’e curious about your own genetics you can get your genome from 23andme and then have it evaluated for metabolism issues such as this by a knowledgeable practitioner. This has become a huge part of my practice and it’s been so profoundly helpful! Contact me to learn more at drbrooke@betterbydrbrooke.com.
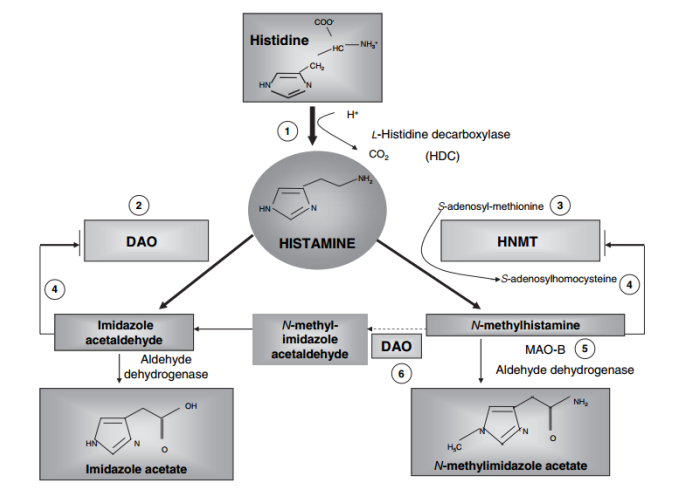
Genes (Thus Enzymes) involved in Histamine Metabolism & Processing Include:
- HNMT– which requires effective MTHFR as SAMe (the main methyl donor in the body and end product of folate and B12 metabolism) is a cofactor for this enzyme. Cofactors are like the gas that make the enzyme go.
- MAOB – which requires vitamin B2 and iron
- NAT2 – which requires vitamin B5 (B5 creates CoA which is the cofactor for NAT2)
- DAO – is the enzyme in your gut that breaks apart histamine that comes in with food or generated from local gut infections and it requires vitamin B6 and copper as cofactors.
Other genetic issues that will impact histamine processing are issues with MTHFR and PEMT.
Back to me as an example it’s no wonder I have histamine issues given that I have issues with MTHFR (and MTRR which is key to B12 metabolism) and thus struggle to fuel HNMT with good amounts of SAMe. But I also have homozygous DAO (I have two bad copies of that gene) meaning I have problems digesting histamine in food. I also have a slow, sluggish NAT2 and a SNP in MAOB so I don’t clear it out of my system very effectively. The slow NAT2 created the super annoying symtpom of irritable bladder, always having to go and never feeling like I was all the way empty. Especially at bedtime when I was getting up eight times to pee before I could even think of staying down for the night.
What happened for me was a variety of factors including a recent uptick in both histamine containing foods and tyramine containing foods (which run through MAOB which caused a backlog of histamine for my other enzymes to process – like my slow NAT2). As well as an increased stress burden and serious sleep deficit this past year.
I was dealing with increased irritability and terrible insomnia as well as vague itching that seemed to come and go so I had a hard time tying it to anything in particular. As well as the frequent urination that was worse at night. I was also looking pretty puffy from the inflammation and vasodilation of all this histamine in my system.
I chalked all this up to stress before I realized what was happening. My digestive symptoms seemed to be hit and miss. This is often the problem with histamine issues in that it can be hard to nail down that it is in fact histamine foods when some days your bucket is less full and you do OK, another day you had more histamine foods and you suffer more. This creates a lot of “but sometimes when I eat that thing I’m OK….so it can’t be that right?” The inconsistency of symptoms makes this often very confusing
And it’s particularly interesting how this relates to female hormones as well. DAO enzyme is naturally bumped up by progesterone so your symptoms may be worse the first two weeks of your cycle but improve as progesterone rises in the luteal phase (2nd two weeks of cycle) and why many of you felt your allergies or food intolerances were gone during pregnancy. This is also an interesting correlation for PCOS as we tend to be overall lower progesterone if we’re not ovulating.
Order Hangry and get some AMAZING bonuses right now!
If you’ve ever felt like a Hangry B*tch and are ready to balance your hormones and restore your joy in just 5 simple steps then Hangry is for you!
GET YOUR BONUSES NOW
When I came off all histamine foods I few other interesting things happened. For one, my cycle in the past has been irregular thanks to PCOS but I’ve had that managed for many, many years however my cramps for the last several years have been worse, not terrible but worse. I chalked this up to being postpartum. But when I got my histamine bucket empty I had zero, like nada none-at all, cramping with my period. In fact it shocked me each time I got a period as it came on with no warning at all – which actually was amazing! No PMS irritability, worsening fatigue and no cramps. I also stopped breaking out so much – again something I had written off lately as just my PCOS and stress.
I also dropped a lot of water weight from lowering the inflammation and as a girl plagued with back, knee and neck injuries I was so thrilled to see my joint pain all but disappear – particularly in my hips and knees. I’d attributed most my recent flare in joint pain to training, being post-baby and still healing my low back, core and pelvic floor after my last baby as well as my lack of sleep.
Looking back now I see histamine playing a bigger role for me in the past as well. Clearly some of my PCOS related symptoms are exaggerated with histamine especially acne and water retention. I also remember my first year at Bastyr where I was under an incredible amount of academic stress as well as going through a divorce.
During this entire year I had horrible hives from literally everything that touched me. I tried every natural remedy, herb and supplement under the sun but finally resorted to daily Zyrtec as I was reacting to my bra, my socks, the plastic suit and respirator we wore during anatomy lab to tone down the formaldehyde exposure, even the tourniquet on my arm when they drew blood trying to figure out what was wrong with me!
For me, this was largely a genetic/sluggish enzyme issue but there are a number of other causes for histamine intolerance including:
- Infections or pathogens (chronic viruses, gut infections like SIBO, etc. as they either produce histamine or can interfere with methylation which plagues enzymes that process histamine and hormones)
- A high protein diet could potentially create this issue as histadine is an amino acid we get from food (protein) and then convert that to histamine
- Increased dietary intake of high histamine foods fermented foods such as sauerkraut, kombucha, kimchi, aged foods such as cheeses and cured meats, leftovers, other high histamine foods like spinach, tomato, avocado, banana.
- Nutrient deficiencies including B12, folate, B6, B2, B1, Zn, Cu, C and methionine
- Antibiotics as they disrupt gut immune balance and
- Antacids directly block histamine release which can cause a build up in your system as because your healthy gut bacteria thrive in an acidic environment. Gut bacteria also contribute to gut immune balance, leaky gut and food sensitivities all of which increase risk of gut infections and overactive gut immunity meaning more histamine.
- Long term antihistamine use as they block histamine release from cells so they build up in your system needing to be processed by your own intracellular processes which can be bogged down from many factors.
- Increased metabolic or nutrient demands due to stress of all types think adrenal fatigue/HPA Axis dysfunction as well as high anxiety, lack of sleep, poor diet, excessive exercise, etc.
- Poor estrogen metabolism due to genetic issues, estrogen dominance in PCOS or various other conditions or from medications such as the pill or HRT
- Alcohol
- Environment high pollen counts, mold, mildew, dust mites, natural gas leaks, etc.
- Gut imbalances such as IBD, IBS, or leaky gut.
What You Can Do About You Histamine Intolerance?
Follow a lower histamine diet. This is job one: stop filling up the bucket. This diet is restrictive, I’m not going to lie but the good news is that if you suspect histamine issues and you avoid it for even just two weeks you will start to see improvement. Get my Histamine Avoidance Diet Handout right here.
A ketogenic diet may be an option too. Learn more about that on this recent podcast with Mike Mutzel, MS. I find most people do well following my Histamine Avoidance Diet but if you’re still struggling you can also keto or at least limiting protein intake and opting for more fat (remember protein contains histidine which converts to histamine).
Heal your gut. Start with a good rotation of probiotics but avoid any that are made via fermentation such as soil based probiotics which are normally great don’t work as well when you have histamine issues. These include Garden of Life Primal Defense, Prescript Assist or Megaspore.
Consider a gut healing product that lessens inflammation and tightens up the gut lining deceasing food reactivity. I’d suggest working with a savvy provider to deal with any suspected or known infections in the gut such as SIBO or any other critter as they will release lot of histamine.
Stress. Manage it from all angles. This will help heal your gut, decrease epinephrine/adrenaline that has to be metabolized by MAO enzymes so they can be available for histamine clearance and start to recover. Remember stress isn’t just in your head, metabolizing cortisol and adrenaline put a big demand on your biochemistry including methylation which if running poorly can increase histamine issues.
Consider adrenal adaptogens and electrolytes as well. Meditate, go for #mantrawalks and do your best to minimize stress where you can. Oh and play! Get a hobby, do stuff just for the fun of it – doctors orders!
Know how you’re methylating. If you have known MTHFR issues or have had elevated homocysteine or any other test indicating you struggle with this fundamental aspect of human metabolism get help from someone who knows how this all interplays. You can also support with creatine and phosphatidyl choline as both are end products of methylation and super important to your health. Phos choline can be found in eggs or taken in supplement form and is part of every cell membrane in your body – big deal right? Creatine bound to magnesium is a great supplement to try as well (less gas and bloating that other forms). Beyond that I suggest getting help with methylation to avoid unwanted side effects and increased health risk.
Mange your allergies. Use dust mite covers on pillows, etc. Clean your air conditioners and air ducts. Dust your home, really well. Get a good air purifier and avoid scented stuff: candles, air fresheners, cleaning products etc. Consider getting rid of carpet.
Supplements To Consider
- DAO enzymes can help you breakdown histamine as it comes into your digestive system.
- Vitamin C can help stabilize mast cells to release less histamine.
- Quercetin can be very helpful for allergy related symptoms but higher doses can also slow MAO enzymes so best to take as needed vs. daily and this is where it helps to know your other genetic issues via something like 23andme.
- Omega threes and phosphatidyl choline are both great for keeping cell membranes healthy and stable as well as helping lower inflammation. Stable mast cells mean less histamine spillage and histamine itself can contribute to inflammation so these both help tremendously.
- Adrenal adaptogens like ashwaganda and electrolytes while you work on managing stressors.
Again though, managing what is coming in and filling up your histamine bucket is paramount to you getting on top of this.
Grab My Low Histamine Diet Here!
Finally, know you can recover from this! The diet aspect can feel hard but if it helps it’s so worth it. You can do it.